Celebrating
International Women’s Day
By Sheila Menon
International
Women’s Day is a celebration of respect, appreciation and love toward women for
their achievements. It is also a time for individual women to recognize their
personal worth as mother’s, daughters and ambassadors of change.Many
women today work; they also cook, manage the domestic economics and wipe runny
noses. It can sometimes feel that the right to go to work simply means having
two full time jobs squeezed into the space of 24 hours. Of
course, 21st century living has an impact on the male population. But
men did not have to fight for the right to go to work or to have a value placed
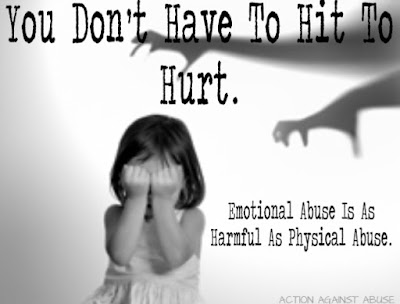
on their dreams. This can result in different perspectives, and sometimes communication
can breakdown between the sexes. Stress builds up, tensions fly and women can
sometimes feel guilty that they are not doing enough. One study suggests that
women measure the amount of housework they feel they should do (or feel guilty
for not doing) by what they observed their mothers doing. Change clearly
starts at home. Women are already contributing to a more equal society when
they share informed thoughts and opinions with their daughters and sons. But
change does not stop here. Children often model what they see making it
important for every woman, married or single to embrace her right to have an
opinion. It is her courage to break with tradition and to speak out or act, which
creates the opportunity for future generations to grow up with a better
understanding of the dynamics of equality.
In 1995 nearly 200 governments signed the Beijing
Declaration and
Platform for Action, which is a historic road map envisioning a world where each
woman and girl can exercise her choices, such as participating in politics, getting
an education, having an income, and living in societies free from violence and
discrimination. Political voices are the vehicle that provide better opportunities for female employment
and safety. But just as important for change to occur is each woman who
everyday celebrates her validity as a person in her own right, because it is from
these small steps that great changes occur.
LCCH invites you to
celebrate International Women’s Day with a series of one-day workshop about
Communication in Families. Registration
fee RM 50 (not inclusive 6% GST).